There has been controversy not only about the diagnosis of ADHD, now refuted (Vidal Gshoda 2012, Jensen 2016, Morgensterns 2016, De Cresenzo 2017, Lopez Pinar 2018) but also its treatment with stimulant drugs. The main concerns were the possibility of people developing drug misuse or diverting stimulant medication (Singh 2008). However, ADHD itself is associated with an increased rate of substance misuse disorder (Elkins 2007, Wilers 2008). Chang et al using the Swedish national registers of individuals born between 1960 and 1998 (about 39,000 people) found ADHD was not associated with an increased rate of substance misuse. They concluded that the data suggested a long-term protective effect on substance abuse (2013). The recent publication of an international consensus statement on screening, diagnosis and treatment of substance use disorder patients with ADHD provides invaluable evidence based guidance (Crunelle 2018).
Notwithstanding this, professionals and practitioners have a responsibility to make clinical decisions appropriate to the circumstances of the individual in consultation with them (NICE 2018). Specifically, for those with ADHD where there is a concern about substance misuse or diversion a risk assessment addressing these issues in particular is recommended. A clinician may choose not to prescribe stimulant medication for specific reasons including concerns about substance misuse or diversion.
An adult who has just received a diagnosis of ADHD is in a very different situation compared to a child with ADHD. The adult has sought the diagnosis so has insight into his/her life being less than satisfactory and, crucially, wishes to change it. Ultimately he/she is hoping for a functional change: psychologically, socially, educationally/occupationally (BAP 2007).
Central to treatment is a discussion with the person on options available and recommended with the person considering:
- If he/she wishes to commit to treatment
- And, if so, which of the options to choose
Following this a jointly agreed individual care plan is drawn up by the ADHD specialist with the person.
Treatment of adults with ADHD should be multimodal (Kolar 2008; Knouse 2008; Murphy 2005; Weiss 2008) i.e. a combination of pharmacological and psychosocial interventions the purposes of which are to reduce core symptoms of ADHD (inattention, hyperactivity and impulsivity and also mood lability) whilst teaching the individual skills and strategies to overcome functional impairments.
The NICE Guidelines (2018) recommend:
- Offer medication to adults with ADHD if their ADHD symptoms are still causing a significant impairment in at least one domain after environmental modifications1 have been implemented and reviewed.
- Consider non-pharmacological treatment for adults with ADHD who have:
- Made an informed choice not to have medication
- Difficulty adhering to medication
- Found medication to be ineffective or cannot tolerate it.
- Consider non-pharmacological treatment in combination with medication for adults with ADHD who have benefited from medication but whose symptoms are still causing a significant impairment in at least one domain.
- When non-pharmacological treatment is indicated for adults with ADHD, offer the following as a minimum:
- A structured supportive psychological intervention focused on ADHD
- Regular follow-up either in person or by phone
Treatment may involve elements of or a full course of CBT.
1 Environmental Modifications :
Environmental modifications are changes that are made to the physical environment in order to minimise the impact of a person’s ADHD on their day-to-day life. Appropriate environmental modifications will be specific to the circumstances of each person with ADHD and should be determined from an assessment of their needs. Examples may include changes to seating arrangements, changes to lighting and noise, reducing distractions (for example, using headphones), optimising work or education to have shorter periods of focus with movement breaks (including the use of “I need a break” cards), reinforcing verbal requests with written instructions.
(NICE Guidelines 2018)
The treatment options will now be described in the following sequence:
- ADHD specific medication
- Treatment of co-morbidities
- Non-pharmacological interventions delivered by the ADHD Clinic
- Other important interventions.
8.1 ADHD Specific Medication
Drug therapy is the first line treatment recommended by NICE (2018) for treatment of adults with ADHD. There is a good evidence base to show the effectiveness of pharmacotherapy. For example methylphenidate, a stimulant; lisdexamfetamine, a stimulant, (Adler 2008); atomoxetine, a non-stimulant, (Adler 2009; Cunill 2013) each has a good evidence base. Cortese (2018 and 2020) gives a good overview of pharmacologic treatment of ADHD.
The updated NICE guidelines recommend that all medication for ADHD should only be initiated by a healthcare professional with training and expertise in diagnosing and managing ADHD (2018).
NICE (2018) has amended its guidance on medication choice to:
- Offer lisdexamfetamine or methylphenidate as first-line pharmacological treatment for adults with ADHD.
- Consider switching to lisdexamfetamine for adults who have had a 6-week trial of methylphenidate at an adequate dose but have not derived enough benefit in terms of reduced ADHD symptoms and associated impairment.
- Consider switching to methylphenidate for adults who have had a 6-week trial of lisdexamfetamine at an adequate dose but have not derived enough benefit in terms of reduced ADHD symptoms and associated impairment.
- Consider dexamfetamine for adults whose ADHD symptoms are responding to lisdexamfetamine but who cannot tolerate the longer effect profile.
- Offer atomoxetine to adults if:
- they cannot tolerate lisdexamfetamine or methylphenidate or
- their symptoms have not responded to separate 6-week trials of lisdexamfetamine and methylphenidate, having considered alternative preparations and adequate doses.
Further medication choices
- Obtain a second opinion or refer to a tertiary ADHD clinic service if ADHD symptoms in an adult are unresponsive to one or more stimulants and one non-stimulant.
- Do not offer any of the following medication for ADHD without advice from a tertiary ADHD service:
- Guanfacine for adults
- Atypical antipsychotics in addition to stimulants for people with ADHD and coexisting pervasive aggression, rages or irritability
- Medication not included in recommendations 1-5
- Medication choice – people with coexisting conditions.
- Offer the same medication choices to people with ADHD and anxiety disorder, tic disorder or autism spectrum disorder as other people with ADHD.
- For adults with ADHD experiencing an acute psychotic or manic episode:
- stop any medication for ADHD
- Consider restarting or starting new ADHD medication after the episode has resolved, taking into account the individual circumstances, risks and benefits of the ADHD medication.
The main ADHD drugs used in adults are licenced for use in children and young people with ADHD, this is not the case for adults or may only apply when the drug has been started in childhood.
The Medical Protection Society’s (MPS) recommendations for prescribing off–label use of medications is helpful and should be followed when prescribing for adults with ADHD. The MPS highlights the following points:
- Ensure the most suitable drug is being prescribed for each patient and that there is no reasonable alternative that has marketing authorisation.
- Be satisfied that there is a sufficient evidence base or experience of using the medicine to demonstrate its efficacy and safety.
- Understand the known attributes of the drug and each doctor’s responsibility for ensuring monitoring and follow up. Record each decision in the patient’s record.
As a first step, there should be an in-depth discussion with the patient outlining the benefits of drug treatment. This should include which drugs are available, potential side effects, the need for a full medical assessment pretreatment and on-going monitoring until a stable dosage has been established followed by an annual review to determine if the treatment should be continued.
Before starting drug treatment, a full medical assessment should be completed in addition to a full mental health and social assessment. The medical assessment should include:
- Full history and physical examination
- assessment of history of exercise syncope, undue breathlessness and other cardiovascular symptoms
- heart rate and blood pressure (plotted on a centile chart)
- height and weight
- examination of the cardiovascular system
- family history of cardiac disease
- current medication
- An ECG is not needed before starting stimulants, unless the person has any of the features listed below or a co-existing condition that is being treated with a medicine that may pose an increased cardiac risk (NICE 2018, amended 2019).
- history of congenital heart disease or previous cardiac surgery
- history of sudden death in a first degree relative under 40 years
- shortness of breath on exertion compared to peers
- fainting on exertion or in response to fright or noise
- palpitations (see NICE 2019)
- chest pain suggestive of cardiac origin
- signs of heart failure
- murmur on auscultation
- blood pressure classified as hypertensive (see NICE 2018 guidance on hypertension)
- Risk assessment for substance misuse and drug diversion.
(NICE Guidelines 2008, 2018, 2019)
The medical assessment would normally be carried out by the person’s General Practitioner with the ADHD Clinic completing the risk assessment for substance misuse and drug diversion.
Drug treatment for adults with ADHD should be initiated by a psychiatrist (with training and expertise in the assessment and treatment of ADHD: NICE 2018). In the UK, nurse prescribers specialising in ADHD can undertake this role. This might be considered for the future as the Clinical Programme becomes established. Methylphenidate, a controlled drug, has recently been licensed for prescription by registered nurses in Ireland (Misuse of Drugs Regulations 2017). The other drugs listed are not controlled drugs so could be potentially prescribed by nurse prescribers (as could methylphenidate) if included in their clinical prescribing agreement (CPA) and signed off by their consultant and the relevant drugs and therapeutic committee.
Typical improvements reported with treatment include less restlessness and fidgeting; improved ability to sustain effort for tedious tasks; improvement in initiating and completing tasks; better concentration for reading and less ceaseless unfocused mental activity.
This Clinical Programme does not include full details on prescribing, contraindications, side effects and adverse effects/warnings for which the reader should refer to the Irish Medicines Formulary (IMF 2018).
Annual Review
Once the patient has been stabilised on medication and has completed the recommended psychosocial interventions, he/she should be discharged to their GP who should continue to prescribe the medication advised by the specialist. However, in line with NICE 2013 Quality Statement Seven on Annual Review of Drug Treatment, this Clinical Programme includes the recommendation that adults with ADHD who are taking drug treatments for ADHD have a specialist review annually to assess their need for continued medication.
Issues to be addressed in this review should include:
- Preference of the individual regarding medication, including stopping or changing it
- An assessment of clinical need (including whether medication has been optimised), benefits and side effects with the patient
- Effect of any missed doses, planned dose reductions, brief periods of no treatment as reported by the patient together with preferred pattern of use
- Effect of medication on existing or new mental health, physical health or neurodevelopmental conditions
- Need for additional psychosocial and occupational supports
- Consider trial periods of stopping medication or reducing the dose when assessment of the overall balance of effects and harms suggests this may be appropriate.
(NICE 2018)
GPs should be advised to prescribe for one year periods subject to the outcome of each annual review.
8.2 Treatment of Co-morbidity
An essential part of assessment is to identify any comorbid disorders and then determine if the symptoms are part of ADHD, a reaction to untreated ADHD or independent of ADHD. If the latter, a clinical judgement based on an assessment of symptoms should be made on which condition to treat first.
Considering each of the common comorbidities in turn:
1. Anxiety symptoms/disorder
Those occurring independently of ADHD should be treated using a psychological approach. Treatment for ADHD can also be started. Of note, atomoxetine has been shown to be effective in ADHD with social phobia (Adler 2009).
2. Mood disorders
Treat the most severe disorder first. If moderate or severely depressed, the treatment of depression is the first priority. Otherwise ADHD may be treated first and associated mood symptoms may also respond.
3. Substance use disorder
Substance use disorder (SUD) and co-morbid adult ADHD is well recognised (Biederman 1995; Faraone 2007; Wilens 2007). There is controversy about the nature of the relationship; whether ADHD leads to substance misuse as a form of self-medication or if the two conditions have the same neurobiological basis.
The College of Psychiatrists of Ireland’s Faculty of Addiction Psychiatry reports little current abuse of stimulants by young people presenting to services. It noted there appears to be little “street” value for these medications. However, it also noted the recent dramatic increase in stimulant use and misuse in the US. It concluded that a well run ADHD service using careful assessments will reduce the risks of misdiagnosis and inappropriate prescription of stimulant medication.
The implications for treatment are that those who are actively misusing substances including alcohol or at risk of doing so are also likely to misuse or divert stimulant medication. It is recommended that the immediate release or modified release stimulants that can be easily injected or insufflated are avoided (NICE 2018). Atomoxetine may be used in this situation and, of note, it has been shown that atomoxetine improved core ADHD symptoms in people with alcohol misuse even if they resumed drinking (Wilens 2008).
Screening for ADHD in young people and adults attending substance use disorder services should be carried out routinely. In line with this, psychiatrists working in these services should be trained in the assessment and management of ADHD. Specific substance use treatment programmes should be available for those with co-morbid ADHD in SUD services (Crunelle 2018).
4. Eating disorders
Bulimia, binge eating disorder and anorexia nervosa bingeing/purging sub type are now known to be associated with ADHD (Biederman 2007, Svedlund 2017). Specific ADHD treatment may impact on the eating disorder. It may be that the ADHD symptoms of impulsivity and executive dysfunction are contributing to or the cause of the underlying disordered eating behaviours. It may also be that depression, anxiety and low self-esteem, common in both eating disorders and ADHD, are relevant (Quinn 2008).
5. Sleep disorders
Whilst there is little research into sleep disorders in adults with ADHD, 70% of children with ADHD report sleep problems. These are characterised by longer sleep onset latency, shorter total sleep time and lower sleep efficiency (Cortese 2009). The theoretical basis for the relationship between sleep and ADHD is the overlap between the cortical and brainstem regions involved in sleep-wake regulation and in ADHD.
Delayed Sleep Phase disorder: The commonest sleep disorder is delayed sleep phase syndrome (DSPD) in which the body clock is several hours behind external time due to a delay in melatonin secretion, an average of 105 minutes in adults and 45 minutes in children with ADHD (van Veen 2010). This leads to falling asleep late, waking up very late and feeling awake late at night. Treatment involves good sleep hygiene, the most important point of which is getting up at the same time every morning rather than the time of going to bed. Melatonin can improve sleep in people with DSPD (Szeinberg 2006, Van der Heijden 2007).
Restless Legs Syndrome (RLS): Up to 44% of people with ADHD may have restless legs syndrome (Cortese 2013). It is important to always enquire directly for RLS (Ferri 2007) particularly since treatment with iron in those with low ferritin can be very helpful.
Obstructive Sleep Apnoea (OSA): 18-65% of children with ADHD have OSA, mostly mild (Cortese 2013). There is very little research on OSA in adults. With mild OSA, a mandibular advancement splint may help the sleep disturbance.
ADHD drugs and sleep: Stimulant ADHD drugs can contribute to sleep problems so advice on not taking them too close to bed time is important.
8.3 Non-pharmacological Interventions to be delivered by the ADHD Clinic
Whilst stimulants and atomoxetine are likely to benefit both the core symptoms of ADHD and other commonly associated symptoms such as mood lability, the complexities of adult life require a multimodal approach (Weiss 2008; Mongia 2012). Interventions most usefully offered include psychoeducation, cognitive behaviour therapy and teaching skills to assist with organising daily activities.
Both ADHD specific medication and non-pharmacological interventions require the person to make important treatment decisions. However, the commitment required for the non-pharmacological interventions is of a substantially greater magnitude. It requires on-going personal investment in terms of engagement and of time; both of which are challenges for a person with ADHD. This means all such interventions must be ADHD friendly by which is meant focused on channelling the positive attributes of ADHD thereby enhancing engagement.
Having reviewed the interventions available and their evidence base (Vidal - Estrada 2012), including their longer term efficacy (Lopez-Pinar 2018), this Clinical Programme recommends two for delivery. These are:
- ADHD specific cognitive behaviour therapy for adults (Young, Bramham 2012)
- Occupational therapy for ADHD in adults (Donoghue 2017: Appendix IV). Each will now be briefly outlined.
ADHD specific Cognitive Behaviour Therapy
The Young-Bramham CBT Programme for ADHD can be delivered as an individual or group treatment. It addresses both the core and associated problems of ADHD in adults covering:
- Psycho-education about ADHD
- Attentional strategies
- Time management techniques
- Problem solving strategies
- Impulse control
- Addressing associated problems
- Positive psychology
The group format has the benefit of providing opportunities to both meet other people with similar problems and share strategies for coping. It is designed in a modular format, each to be delivered over six weeks. This allows the therapist to choose the modules appropriate to the needs of the group. The programme modules are:
Core Problems
- Attention
- Memory
- Organisation/ time management
- Impulsivity
Associated Problems
- Interpersonal relationships
- Anxiety
- Frustration and anger
- Low mood and depression
- Sleep
- Substance Misuse
Cognitive behaviour therapy specifically for ADHD provides:
- psychoeducation
- training in concrete skills e.g. organisation and planning
- together with outside practice to encompass maintenance of these skills in daily life (Young and Bramham 2013).
Its role is to provide a structured short-term therapy in which an individual:
- Gains insight into ADHD and how its effects can be reduced by focusing on strategies to overcome areas impacted on. In this context it is also important to identify:
- the individual’s strengths, skills and talents
- emphasise the promotion of lifestyle changes and targeted strategies.
- Develops organisational and planning skills such as:
- time management
- diary keeping (including especially by mobile phone)
- planning tasks as a series of smaller achievable steps to overcome distractibility, feelings of being overwhelmed and problems with task initiating.
- building rewards into the system to sustain focus on task.
- Completing homework as an integral component of developing the skills of self-regulation.
To ensure maximum access, this Clinical Programme recommends ADHD specific CBT be provided in group format. This has been shown to be effective clinically and economically (Solanto 2011).
This is in line with the NICE Quality Standards for ADHD (2013) which recommends that children and young people with moderate ADHD are offered a referral to a psychological group treatment programme. Whilst NICE has not set this quality standard for the treatment of adults with ADHD, its updated guidelines now recommend a structured supported intervention focused on ADHD which may offer elements of or a full course of CBT (2018). This together with the positive evidence on psychosocial approaches in adults with ADHD indicates it is appropriate to offer adults such treatment.
Occupational Therapy for ADHD in adults
Occupational therapy may improve functional outcomes and quality of life for adults with ADHD (Gutman and Szczepanski 2005). The treatment approach is person centred, individualised, recovery focused and targets functional outcomes.
Skills training, sensory modulation interventions, lifestyle redesign, cognitive assistive technology, psychoeducation, compensatory strategies/ environmental adaptations, social skills training and activity scheduling are specific interventions that are utilized (Gutman and Szczepanski 2005). These interventions can be delivered in a group format or on a one to one basis. For instance monitoring and regulating sensory stimulation (over- and underload) through a sensory diet can improve attention, help develop skills to organize the physical environment, could improve performance in the workplace and social skills training could enhance social functioning (Gutman S, Szczepanski OTR, Szczepanski M. 2005).
The OT intervention briefly outlined below is recommended because it is task focused and delivered individually and so it would suit people who prefer these approaches (Donoghue 2017: Appendix IV). The intervention is based on the core occupational therapy principle of helping people to do the everyday things that they want to do and need to do. It targets sensory modulation (as a means of sustaining attention) and executive functioning.
- Sensory modulation: by identifying the sensory modulation patterns of the individual with ADHD the occupational therapist (OT) can devise sensory strategies to help focus attention.
- Executive function is improved by working with the person “to organise to get organised”.
In providing a bespoke suite of measures to improve attention and executive function, each individual acquires the skills to do his/her necessary everyday tasks.
The link for both the CBT and OT interventions is given in Appendix IV.
8.4 Other important interventions
These interventions are seen by the Clinical Programme as important contributors to the overall care plan of each adult with ADHD. They complement those provided by the ADHD Clinics and may be used simultaneously with the ADHD Clinic interventions or subsequently, depending on the person’s needs and preference.
Voluntary ADHD Organisations in Ireland
There are a number of ADHD organisations in Ireland.
These are:
- ADHD Ireland is the largest of the organisations and is expanding its activity outside Dublin.
- ADHD Cork originally founded by HADD Ireland but now a separate body providing services for Cork.
- Friends of Autism and ADHD which provides supports in the North County area of Dublin.
Of relevance to this NCP, ADHD Ireland provides or is in the process of developing the following services for people over 18 years of age:
- Adult support groups which run 3/52 weeks
- Recruiting volunteers so it can set up peer-to-peer adult support groups around the country. Groups now running in Sligo, Galway, Bray with a new group starting in Cork shortly.
- Plans are well advanced to develop an app outlining services and supports for adults with ADHD.
- Currently trialling an online support group in partnership with Turn2me.
- Conferences for adults.
- Advocacy via media
- Well established parenting courses and is planning training courses for adults with ADHD in the future
- Support line with 1 in 2 calls from adults needing information on where to get a diagnosis. Received approximately 1,000 calls in 2019.
It is recommended that each adult diagnosed with ADHD is informed of the adult support groups and webinars provided by ADHD Ireland and encouraged to link in.
ADHD specific coaching
ADHD specific coaching is based on the principal that every adult with ADHD has a different version of ADHD. Each person has a different set of symptoms and experiences each symptom to a different degree. Frequently there is at least one co-morbidity. Learning style, personality type and working style all add to the complexity of working with the person. Because each adult with ADHD is unique, one-to-one coaching can be an effective way of supporting people to meet their full potential and live their best life.
ADHD coaches need to have a combination of coaching skills and in-depth knowledge of ADHD. It is also desirable that they have some knowledge of typical co-morbidities. The coaching partnership is a collaboratively developed, purposeful relationship between a trained coach and a client founded on trust and mutual respect and created and sustained for the sole purpose of reaching the person’s identified, meaningful goals. While the coach may offer information or coaching tools, coaching is not advice, therapy or counselling. The person is viewed as the expert in their life. When a person needs therapy, the coaching process is put on hold until he/she is ready to engage in the coaching process again.
ADHD coaching provides support, structure and accountability to the person (client). Coach and client collaboratively explore strengths, talents, tools and new learning to increase self-awareness and personal empowerment. Together they design strategies and actions and monitor and celebrate progress. They create accountability in line with the client’s goals and aspirations. Coaching is an ongoing process and would typically continue for a minimum of 6 sessions or over a period of at least three months to allow for meaningful change to occur. Having said that, every client is different, some work at a slower pace than others especially where symptoms are severe or there are co-morbidities.
As part of an integrated and multidisciplinary approach, coaching can be recommended as a intervention option. It is useful for the coach to have access to the assessment report (with the person’s written consent) so that the coach has knowledge of the areas identified during the assessment that the client needs to work on. If the client needs CBT or other therapy the client usually engages in that prior to coaching. If the client opts to take medication, it is preferable for the client to wait until they are settled on the right medication and the right dose before engaging in coaching. Where medication is not a suitable option for the client or where the client does not meet the full criteria for a diagnosis, coaching may be a useful option open to them.
General Wellbeing
NICE guidelines on ADHD state healthcare professionals should stress the value of a balanced diet, good nutrition and regular exercise (2008).
Diet: Whilst there is no evidence of benefit from either dietary restrictions or fatty acid supplementation, a well-balanced diet rich in protein and complex carbohydrates whilst minimising sugar intake is recommended (NICE 2016).
Exercise: There is now evidence to suggest that acute exercise (20 to 30 minutes) can enhance executive function. This is based on a meta-analysis of nineteen studies on the effects of physical exercise in pre-adolescents (6-12 years), adolescents (13-17 years) and young adults (18-35 years) (Verburgh 2014). This finding is relevant in adults with ADHD given their recognised difficulties with executive function (Young, Bramham 2012).
Hence a well-balanced diet together with regular exercise is recommended.
Employment
Difficulties in obtaining employment, functioning at work and sustaining ongoing employment are commonly associated with symptomatic ADHD in adults (Asherson 2005, Kooij 2010, Bramham 2016). In Ireland the Department of Employment Affairs and Social Protection funds specific services to provide employment support for people with a health condition, injury, illness or disability. This nationwide EmployAbility Service is delivered locally through a network of offices to ensure ease of access. The functions of each EmployAbility Service are to:
- provide employment assistance and access to a pool of potential employees with varying levels of skills, abilities and training
- provide ongoing support for both the employer and employee throughout the employment
- provide a professional role matching service to help ensure successful recruitment
- provide advice and information on additional employment supports.
The list of local services is available on www.welfare.ie.
Anecdotally, local services appear to vary from being very aware of and helpful to adults with ADHD to being somewhat less aware.
As part of the implementation of this Clinical Programme a link will be established with the Department of Social Protection to ensure the provision of employment supports for adults with ADHD is required of each local EmployAbility Service.
Monitoring Progress
The WEISS Functional Impairment Rating Scale – Self Report (WFIRS-S) is a useful scale in targeting areas for treatment and monitoring progress (Appendix III). The Clinical Programme recommends its use to measure outcomes of treatment.
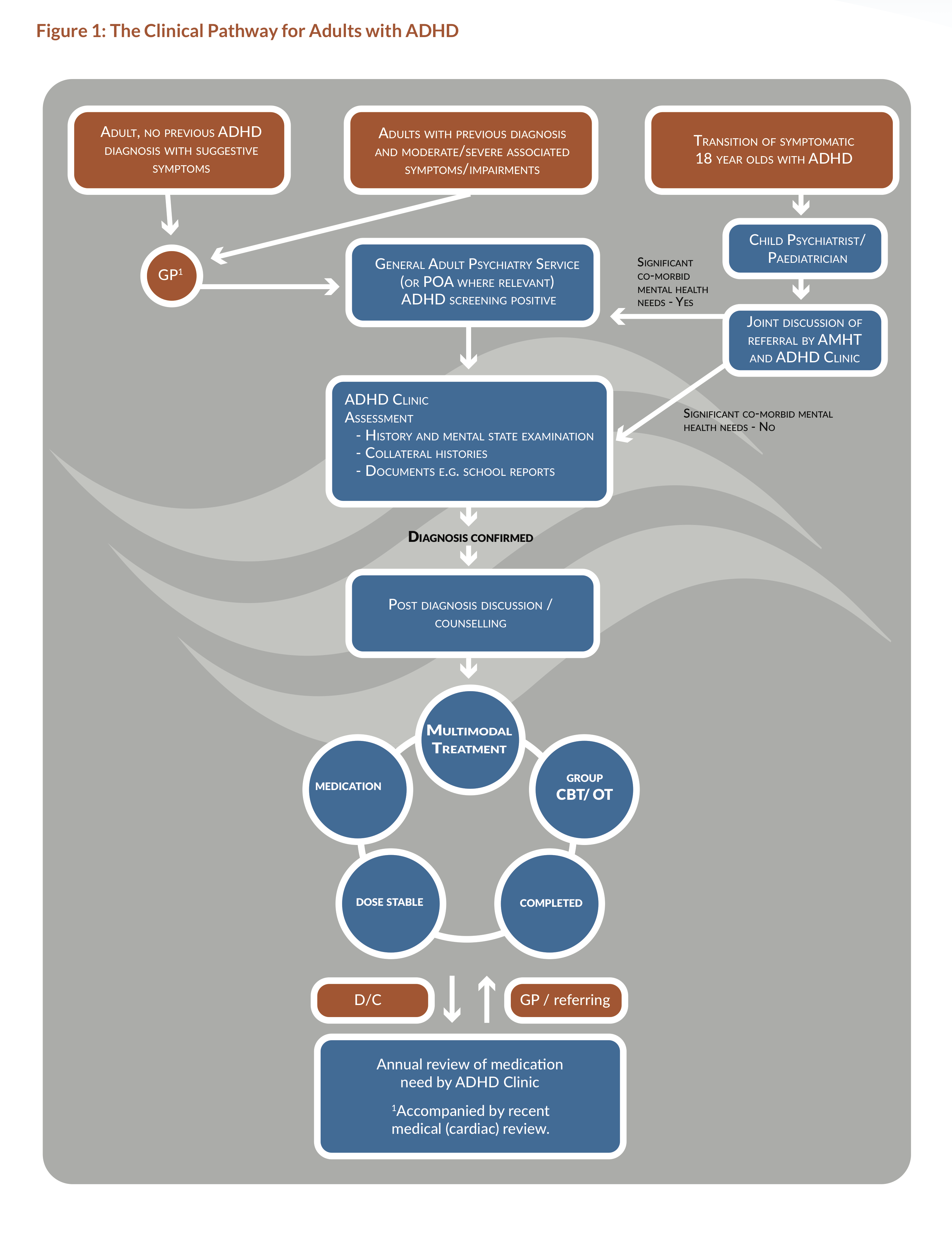
Clinical Pathway
The clinical pathway described in the previous chapter and in this chapter on the assessment process and treatment respectively is shown diagrammatically in figure 1.