The rationale for developing a National Clinical Programme for ADHD in Adults is based on two pillars of evidence: clinical and economic together with evidence from prisons and on mortality.
Clinical Evidence
The adverse consequences of moderate to severe difficulties arising from persistent syndromal ADHD in adulthood are now well recognised (Asherson 2005, Kooji 2010). The three core features of the disorder are inattention, hyperactivity and impulsivity (DSMV:APA 2013). The symptoms related to inattention are those most often complained of and these include forgetfulness, difficulties in organisation particularly of routine tasks, being easily distracted by thoughts or external events. Hyperactivity is less evident in adults but some symptoms may be present such as fidgeting, picking at fingers, tapping hands and feet or playing with hair etc.
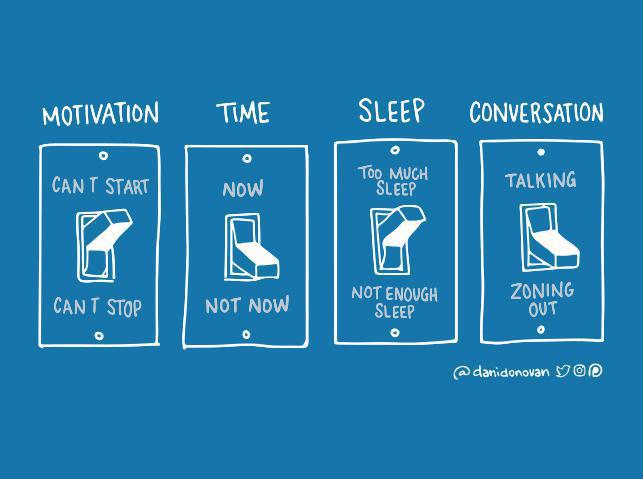
Also common are reports of finding it difficult to sit and listen at lectures or meetings. Talking excessively may occur reflecting difficulty in maintaining concentration on what other people are saying. Like hyperactivity, impulsivity may be less evident but still causes difficulties e.g. in conversation with constant butting in, indiscreet comments and in a documented increase in driving offences (Barkley 2007). Persistence of impulsivity and hyperactivity is seen in adults with ADHD with addiction or forensic problems (Huntley 2012).
The impact of these symptoms is seen in functional impairments and to make a diagnosis of ADHD impairment should be present in at least two of the domains listed below (APA 2013):
- Work or occupation
- Leisure and recreation
- Social interaction
- Relationships
- Management of money
- Driving
- Offending behaviour
The core symptoms of ADHD are dimensional rather than categorical and hence it is important to make a diagnosis of syndromal ADHD in which there is moderate to severe impairments in two or more functional domains. Moderate/severe could be interpreted as repeated job losses, repeated or consistent academic failure, repeated relationship breakdown etc due to the symptoms of ADHD. It is for this group of adults with ADHD that the Clinical Programme is designed.
There are a number of other symptoms that are characteristic of adult ADHD but not included in the diagnostic criteria (Young & Bramham 2007, Barkley 2008, Seli 2015). These symptoms include procrastination, low tolerance or frustration, mood lability, low self-esteem, insomnia, spontaneous mind wandering and needless worrying. As previously outlined, it is mood lability and anti-social behaviour specifically which lead to misdiagnosis if ADHD is not specifically considered as one of the differential diagnoses for adults with nonpsychotic mental health symptoms.
Finally, it is known that comorbidity with other mental health diagnoses is the rule rather than the exception in adult ADHD (Kooij 2001; Biederman 2007; Secnik 2005) with 85% showing such symptoms (Cumyn 2009).
These symptoms may represent core ADHD symptoms, the consequences of ADHD (including self-medication with alcohol and other substances) or a separate comorbidity. The comorbidities include anxiety, depression, substance/alcohol misuse, sleep disorders and personality disorders. Recognition of whether the comorbidities are core or separate in any individual is important in determining appropriate treatment (BAP 2007).
If adults with ADHD do not have access to assessment or are misdiagnosed and do not receive effective treatment, they suffer unnecessarily as do their families and work colleagues. Their impairments, secondary to ADHD, affect them in the listed key domains. Despite this, a recent longitudinal study on clinical service use in young adults (up to 24 years) with ADHD revealed the main determinant of health service use was age rather than need (Eklund 2016).
Research has shown that combined therapy using medication with psychosocial interventions (multimodal treatment) is the most effective way to deal with the core symptoms of ADHD and the resulting impairments (Kolar 2008; Knouse 2008; Murphy 2005; Weiss 2008).
Economic Evidence
The economic argument for treating ADHD in adults is obvious when considered in the context of the broad WHO framework’s (2000) three fundamental objectives of every health system:
- to improve the health of the population
- to respond to people’s expectations
- to provide financial protection against the cost of ill health
The direct and indirect costs and benefits of treating ADHD in adults were summarised by Adamou (2010):
- The tangible and direct costs and benefits of successful treatment of ADHD in adults saves on future medical expenses due to traffic and other accidents; treatment of sexually transmitted diseases; visits to doctors.
- The indirect but tangible costs and benefits of working time gains of health professionals.
- The direct but intangible costs and benefits of reduced suffering for adults with ADHD and their families: also for society as a whole from associated impairments and criminality.
The true economic burden of ADHD in adults was explored in a UK/Danish study reported at the 5th World Congress on ADHD in 2015. This study compared adults with ADHD to their unaffected siblings and controlled for co-morbid diagnoses using the Central Person Register in Denmark.
5331 adults diagnosed with ADHD were identified and when matched with a sibling with no psychiatric disorder yielded 365 pairs.
Combining public and private services, the cost to society was estimated as €13,608 per person per year (Daley 2014).
This is likely to be an underestimate since it does not include the cost of associated co-morbidities which are the norm in adults with ADHD.
ADHD and Prisons
A meta-analysis of the prevalence of ADHD in the prison population gives a prevalence of 31% for men derived from 22 studies based on diagnostic interviews by clinicians rather than just screening. The equivalent figure from women in prisons is 22% based on 8 studies giving an overall rate of 25.5% (Young 2014). This is ten times greater than the prevalence in the general adult population.
Dalsgaard’s study (2013) on the long-term criminal outcomes of children with attention deficit disorder in Denmark showed that children with severe ADHD have a higher risk of criminal convictions in adulthood. This study used the Danish National Crime Register to identify rates of conviction in 206 children (191 boys and 25 girls) treated for ADHD with medication between 1968-1989 and followed up until the year 2000 when their mean age was 31 years. 47% had a criminal conviction compared to the 5.6% rate in the general population i.e. an 8 times increased risk. Co-morbid conduct disorder in both girls and boys increased the risk but the rate was still high at 26% in children with no conduct disorder. The overall rates in boys with ADHD was 47% compared to 7.5% in the general population with equivalent figures for girls being 24% and 1.3%.
A study in a Swedish high security prison with long-term male inmates found a prevalence rate of 40% (Ginsberg 2010). Also found in this study was that all the men with ADHD reported lifetime substance use disorder, most commonly amphetamine, half had mood and anxiety disorders, one quarter autism spectrum disorder. Almost all had antisocial personality disorder preceded by conduct disorder though only 2 out of 30 men had a diagnosis of ADHD in childhood. Psychological assessment revealed executive dysfunction with impaired working memory even when controlling for I.Q.
Ginsberg et al then carried out a 52 week trial of treating these same men with OROS-methylphenindate. 25 of 30 men completed the trial. Medication was found to be very effective in reducing ADHD symptoms, improving global and executive functioning, behaviour and quality of life. No misuse of ADHD medication was detected (Ginsberg 2012). Of most interest, a further long-term treatment outcome study on the same group of prisoners described as a three year naturalistic follow-up continued to show overall improvement (Ginsberg 2015).
Specifically, 15 of 20 people in this study had been released from prison of whom 10/15 (67%) were in employment, usually full-time. There were substantial improvements in ADHD symptoms, global symptom severity and functioning and quality of life maintained after 4 years treatment with methylphenidate. There was a reduction in re-offending with 40% reporting this compared to the expected rate of 70-80%. The average dose of methylphenidate was 144 mgs suggesting that ADHD with concurrent SUD might require higher methylphenidate doses then recommended by the NICE guidelines (2013).
A recent report by the Centre for ADHD Awareness, Canada summarised the benefits in personal, social and economic terms of recognising and treating those with ADHD in the Criminal Justice system (2016).
ADHD and Mortality
ADHD is associated with an increase in mortality as shown in a Danish population based study with an up to 32 year follow up of children, adolescents and adults with ADHD (Dalsgaard 2017). The mortality rate was higher in those diagnosed in adulthood. It remained higher even when adjusted for the co-morbidities of oppositional defiant disorder, conduct disorder and substance use disorder but was then higher in women than men. The excess mortality was mainly related to accidents.
Another large population based study in Sweden examined the rate of serious transport accidents in people with ADHD and the effects of medication on the rate (Chang 2014). In men with ADHD 6.5% had at least one serious accident in the 4 year follow up period compared to 2.6% of men in the general population. The figures for women were 3.9% and 1.8% respectively. During ADHD specific medication periods (20% of the 4 year follow up period), the rate of accidents reduced by 58% with 41% of accidents attributed to non-medication. This effect was seen in both young and middle-aged men. No such effect of medication was found for women. Visual inattentiveness and impulsiveness are suggested as the major contributors to transport accidents in adults with
ADHD (Jerome 2006).
Increased risk of both attempted and completed suicide was identified in a population based study in Sweden (Ljung 2014). The study also showed a pattern of increased familial risk suggesting shared genetic factors are important. It concluded people with ADHD and their families should be targeted by suicide prevention and intervention programmes.
Conclusion
All the evidence outlined in chapters 2 and 3 justifies the imperative to ensure adults with ADHD in Ireland, including those who transition from CAMHS, have access to assessment and treatment within adult mental health services. The focus at this level (secondary care mental health service) will be on those with syndromal ADHD with moderate-severe functional impairments. In line with all other disorders, those with milder forms of ADHD should receive care from primary care services, non-healthcare statutory services such as employability or non-statutory services such as coaching.